Combat Arts Foot Injuries Overview
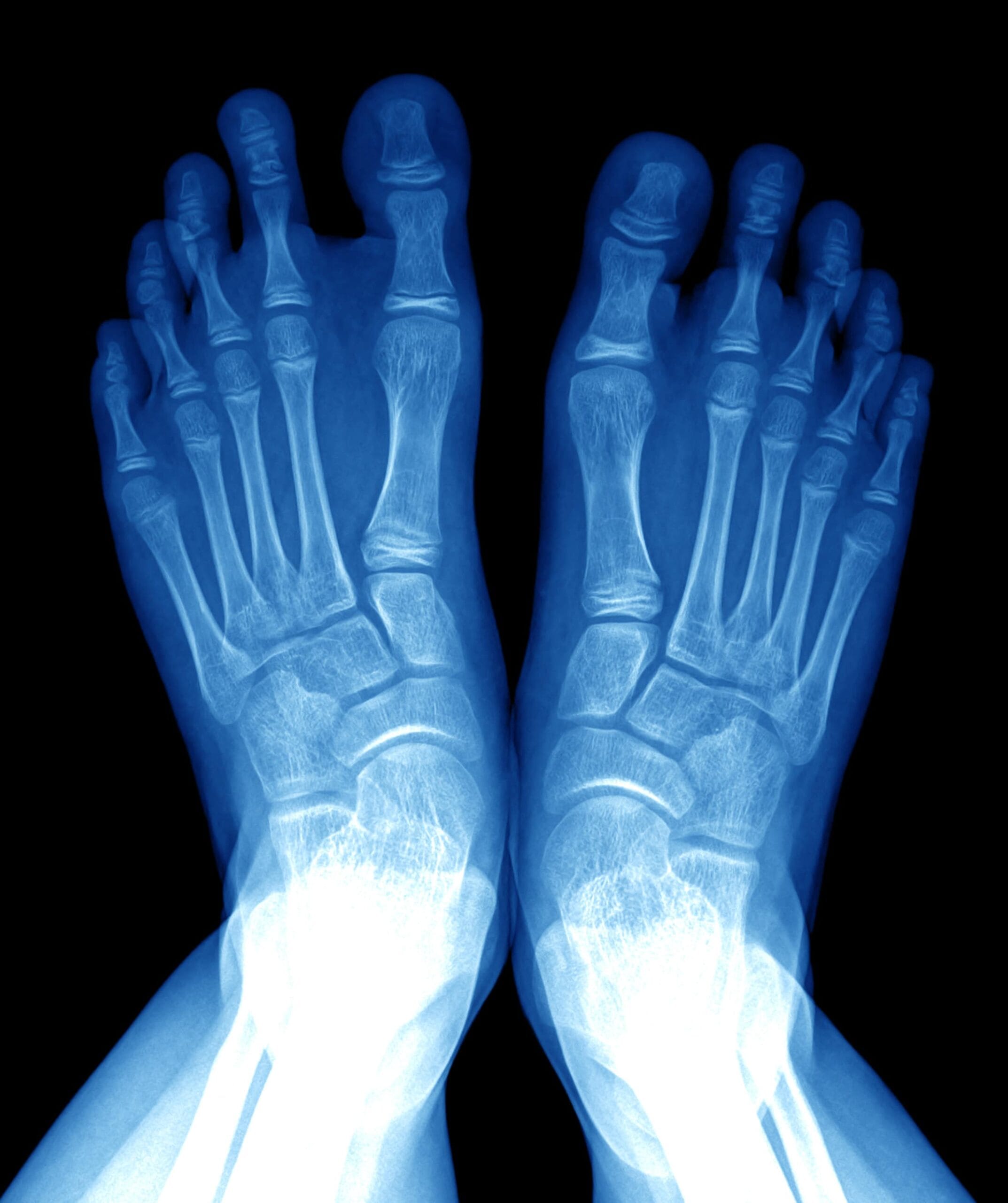
The human foot provides the body with structural strength, movement foundation, shock absorption, locomotive power, and contains 30 joints, 28 bones, and over 100 ligaments, tendons, and muscles. One-quarter of all the bones of the entire human body is found in the feet. Medically speaking, the ankle is part of the foot, although most people refer to them as unique parts.

The foot is comprised of three parts which include the hindfoot, midfoot, and forefoot.
Hindfoot has three joints that link the foot through the ankle or talus. The talus creates a hinge that allows the foot upward and downward motion by connecting to the tibia and fibula. The heel bone, the largest bone in the foot, is the bottom of the heel bone and protected and cushioned by a pad of fat.
Midfoot forms the arch of the foot, absorbing shock and pounding during movement, includes five tarsal bones that are connected to the hindfoot and forefoot by the arch ligament or plantar fascia and muscles.
Forefoot includes the five toes or toe phalanges that help provide flexibility, strength, and movement. The forefoot helps keep the pressure on the ball of the foot evenly balanced. This area supports half of the body’s weight. The toes are particularly prone to injury because of their many small bones and primary position in movement propulsion and supporting the body’s weight.
Former Strikeforce Heavyweight Champion Alistair “The Demolition Man” Overeem holds world titles in both MMA and K-1 kickboxing simultaneously and is interim DREAM Heavyweight Champion. Overeem is also a fighter who was temporarily sidelined because of severe injury to his toe.
Foot Injury Causes
Issues with the feet may result in problems elsewhere in the body, such as pain in the hips, back, or legs. Conversely, problems, or weaknesses in other parts of the body will often affect the feet. For instance, when hip abductors, psoas, or back muscles are weak or injured, often the feet will respond to these issues with pain, gait problems, bunions, hammertoe, or other difficulties.
Foot pain may occur because of structural issues in joints, ligaments, tendons, fascia, muscles, or bones, be referred pain from a pinched nerve in the back, neck, or hip, or may occur because of systemic diseases such as diabetes. Causes include stress fracture, toe injury, plantar fasciitis, bunions, heel spurs, heel pain, and Achilles tendinosis. It is essential to consult with a health professional or foot specialist when foot pain occurs and especially when it is ongoing.

Foot Injury Symptoms

Types of Foot Injuries
Since the foot is composed of many bones, and a host of ligaments and tendons, any number of the structures are prone to injury. It also bears all the weight irrespective of the type and speed of motion. Some of the injuries could be due to acute injuries, others due to chronic wear and tear. This repeated wear can lead to degenerative changes in the fascia and tendons. Some of these injuries include Plantar fasciitis, bunions, metatarsalgia, and heel spurs.
Something as Small as a Foot Injury Limit Your Combat Goals
Sign up Today to Prevent Those Troublesome Injuries!
Related Injuries
This is a repetitive strain injury to the feet that creates persistent pain in at the bottom of the feet. Pain from plantar fasciitis is typically felt in the arch of the foot due to damage or overuse of the plantar fascia. The foot has a thick, wide fibrous band of connective tissue called fascia that stretches from under the heel to the front of the foot, spanning the arch of the foot, and helping to support the arch. This is the plantar fascia or plantar aponeurosis, and it is strong like a ligament, connecting bones at the heel of the foot to bones at the front of the foot.
These tissues are made up of three segments originating at the base of the heel bone. The middle section provides shock absorption to the foot while running and base support when standing. Martial artists may develop pain in all three sections, but typically, it is this center fascia that becomes most tender and painful.
Causes
The causes of plantar fasciitis or plantar fasciosis are not completely understood, but appear to be the result of overuse and repetitive over-stretching of the fascia which creates tiny tears on the surface of the tissue, resulting in deterioration, “collagen degeneration,” Khan et al wrote, and pain where it attaches to the heel bone. It was originally thought to occur from inflammation in the tissue and was called plantar fasciitis since “itis” means inflammation.
The pain is from deterioration of the tissue due to overuse, now referred to as plantar fasciosis. In 2003, Lemont et al looked at 50 cases of plantar fasciitis and found so little evidence of inflammation that they declared plantar fasciitis “is a degenerative fasciosis without inflammation, not a fasciitis.”
Symptoms
The primary symptom of Plantar Fasciitis is arch pain. The pain usually feels like a sharp stabbing, hurts across the full foot, and often pain is most intense when first getting up in the morning or after sitting for long periods.
To learn how Plantat Fasciitis is diagnosed Click Here
The main difference between plantar fasciitis and heel spurs lies in the source of the pain. Pain from plantar fasciitis is typically felt in the arch of the foot due to damage or overuse of the plantar fascia. Heel spurs develop as a secondary result of plantar fasciitis and the pain from heel spurs is localized to the heel of the foot.
Heel spurs are calcium deposits on the heel bone resulting from extreme repetitive stress through pounding, walking, running, kicking, or intensive, incorrect pulling from injured tendons and ligaments.
Symptoms
Pain and sensitivity to touch are the most common symptoms, but some people may be asymptomatic. The pain comes from irritation of the soft tissue around the calcification area. The pain may feel achy or like a knife or pin sticking into the bottoms of the feet. Often the pain eases after movement and is typically due to inflammation.
Causes
Martial artists who run, jump or kick repeatedly may cause heel trauma which incites the body’s healing mechanism to produce bone or heel spurs. Heel spurs usually occur when there is already chronic pain experienced through the heel or foot arch because of chronic inflammation, thickening, and microtears of the connective fascia tissue resulting in plantar fasciitis.
To learn how Heel Spurs is diagnosed Click Here
This is a general term meaning pain in the ball of the foot. The metatarsals are the long bones that connect the foot to the ankle. When a martial artist has metatarsalgia it means the nerves between the metatarsal bones are inflamed, such as from kicking boards. The body weight is balanced through this area by many small bones that may cause simple discomfort up to extreme pain when out of balance or injured.
Typically, the pain will be worse while on the feet and moving. It may hurt to flex the toes and feel pain when wearing shoes, socks, or other gear that surrounds and applies pressure on the foot. Pain may be felt in the ball of the foot when running, jumping, kicking, and other physical activities.
The primary symptoms typically felt in the ball area of the foot include:
Metatarsalgia or pain in the ball of the foot may occur while throwing a much heavier opponent or powerful BJJ takedown, or doing high tornado kicks and landing incorrectly on the ball of the foot creating bone bruises and harming metatarsal nerves. Any overuse, trauma, or injury to the foot may cause metatarsalgia. Examples include:
To learn low Metatarsalgia are diagnosed Click Here
A bunion is a deformity or hard bony bump that forms typically at the base of the first MTP joint or big toe on the inner edge of the foot, although bunions may also develop on the fifth MTP joint or little toe MTP joint on the outside of the foot. The MTP or metatarsophalangeal joints are located at the base of the toe and connect the first metatarsal toe bones to the foot bones. These MTP joints help hold and distribute weight when the body is standing or moving. MTP joints have a thin joint capsule which surrounds them, and ligaments which connect and support them. The first MTP joint or big toe joint is the most prone to developing bunions.
A bunion develops when the first metatarsal bone of the foot starts to shift its position from straight forward to angle off to the side. The big toe then leans into and presses against the other toes which cause an unnatural and painful angling of the joint. A bunion usually feels painful from the beginning and becomes progressively more so as the protruding bone increases in angle and size due to swelling, restricting the movement of the toe, foot, and body.
As a bunion increase in size, it also increases pressure upon other toes and may inflict damage at this primary juncture. Pressure on bones, ligaments, and tendons in this area can impair the foot's functioning and create a condition called hammer toe, or the bursa, which are cushioning fluid-filled sacs or pillows between joints may become sore, inflamed, or infected.
Martial artists, whose feet are constantly stressed from kicking, standing, running, jumping, or moving on the feet for long periods are susceptible to developing bunions. They are also likely to develop bunions because of physical stress placed on feet from repetitive movement, pounding, and often badly fitting shoes. Most shoes don't allow sufficient room for a bunion and place added pressure on the swollen and misaligned joint, increasing pain and promoting further deformation of the area.
Bunions also run in families because certain foot shapes, for example, narrow or wide feet, foot structures such as high or low arch, the shape of the metatarsal head on the toe joint, long or short toes are all hereditary, and some types develop bunions more easily than others. Feet that have loose joints and tendons, long toes, flat feet, low arch, and certain other characteristics are more likely to develop bunions. Bunions may develop from obesity, as well, since excess weight places pressure on the toe joints.
To learn how Bunions are diagnosed Click Here

Common Injuries
In our Common Injuries section, we discuss common injuries such as foot sprains and contusions.
Foot Injury Diagnosis
Various tests and special exams are needed to diagnose foot injuries. Imaging supplements the physical exam and confirms the diagnosis.
Injury Specific Diagnosis
Physical Exam
Doctors will try to reproduce the pain by palpating the plantar medial calcaneal tubercle. They will also try to reproduce the pain with passive dorsiflexion of the foot and toes. This passive dorsiflexion of the first MTP joint is known as the windlass (or Jack's) test.
It is considered a positive test if there’s pain. The doctors will examine gait and look for fat pad contusions, fat pad atrophy, stress fractures, and nerve entrapments.
Imaging
Plantar fasciitis is a clinical diagnosis. Imaging is not required. Yet, plain films are done to evaluate other injuries. This is especially if the injury persists. X-rays and ultrasound evaluations show calcifications in the soft tissues or heel spurs.
An ultrasound will also show thickening and swelling of the plantar fascia. MRI is only requested if conservative therapy fails. It can visualize tears, stress fractures, or osteochondral defects.
Lab Tests
Blood tests are not required to diagnose plantar fasciitis.
To learn how Plantat Fasciitis is treated Click Here
Physical Exam
Doctors will view the foot first and check for any swelling, atrophy, lack of sensation, and skin tears. They will examine the range of motion of the ankle and foot. They will check the gait, arches of the foot, atrophy of the heel pad, and foot alignment. They will palpate the plantar fascia, spurs, tenderness to them, and aggravation by bearing weight. Muscle strength is tested and exams specific to the calcaneus are done. Once such an exam is the calcaneus squeeze test. This is a test where a compressive force is applied to the calcaneus. If pain is reproduced, then the test is positive.
Imaging
Calcaneal spurs are diagnosed with plain films, CT, and MRI. They appear as bony projections that are seen either at the origin of the plantar fascia or the insertion of the Achilles tendon.
Lab Tests
Blood tests are not required to diagnose calcaneal spurs.
To learn how Heel Spurs is treated Click Here
The doctor will evaluate the plantar foot and evaluate the callus areas where there is an increase in foot pressure. They will check the arch of the foot. The metatarsals are evaluated during the gait cycle as well. The calf muscle is examined for tightness.
The diagnosis is confirmed by combining physical examination and imaging. The imaging includes ultrasound and MRI. MRI can provide a detailed image of soft tissues and any early osteophyte changes.
Lab tests are not necessary to diagnose metatarsalgia. The physical exam combined with imaging is necessary to diagnose it.
To learn low Metatarsalgia are treated Click Here
In the physical exam, doctors will look for the deformity and evaluate if it has subtalar joint stiffness, subtalar joint stiffness, midtarsal joint stiffness, resting calcaneal stance position, and tibial torsion. They will also look for any forefoot varus. They have to identify if the deformity is non-weightbearing or weightbearing. They will assess the position of the hallux, compared with the second toes. They will look for any lateral deviation of the MTP joint.
The ROM of the first MTP joint range of motion is assessed. The quality of the joint is assessed whether it has pain or not. Then its axis of motion is checked. The first MTP undergoes two assessments; resting position and range of motion and the second is mobility.
Weightbearing deformities are visible. They are accompanied by increased hallux abduction, increased medial prominence, MTP joint dorsiflexion, hallux purchase, and metatarsus varus.
The diagnosis is usually made by a physical exam. Imaging will identify the extent of joint damage. The imaging is done by plain films with X-rays (AP and lateral weight-bearing) of the foot. Imaging displays lateral hallux deviation at the first MTP. This guides the treatment procedure.
The classification of the valgus is mild, moderate, and severe. It is based on the films obtained through the weight-bearing anteroposterior, lateral oblique, lateral, and sesamoid axial views. These views also help view the structural status of the foot.
The AP projection assesses all the angles, the hallux rotation, and the condition of the first MTP joint.
The lateral projection assesses the position of the joint and dorsal osteophytes. The lateral oblique projection evaluates the trabeculation and projection of the bone. The sesamoid axial view assesses the degenerative joint changes.
Imaging provides the Degree of the Hallux valgus angle (HVA) / Intermetatarsal angle (IMA)
Normal: <15⁰ / 9⁰
Mild: 15-30⁰ / 9-13⁰
Moderate: 30-40⁰ / 13-20⁰
Severe: >40⁰ / > 20⁰
If doctors suspect osteomyelitis, MRI, and radionuclide imaging is done. However, this is very rare.
Lab Tests
Lab tests are not required for HV deformities. However, if metabolic conditions are suspected then Rheumatoid factor, ANA, CRP, ESR, uric acid, and CBC.
To learn how Bunions are treated Click Here
Common Diagnoses
Learn more about how foot injuries are diagnosed and confirmed in our Common Diagnoses section.
Foot Injury Treatment
There are various treatments used to treat injuries in the foot. A vast array of therapies to treat the fascia, the bones, the ligaments, and tendons. The cornerstone of every therapy is a good physical therapy program which includes stretching, condition, and strengthening.
Injury Specific Treatment
Emergency
Plantar fasciitis is not a medical emergency. The pain is excruciating enough to make it feel like it is. The first step is managing the pain.
Medical
The offending activity must stop. Relative rest is advised. Ice and topical NSAIDs are used for pain management.
Other alternatives like deep friction massage of the arch and insertion are beneficial. Shoe inserts or orthotics and night splints are also recommended. Stretching and rehabilitation of the plantar fascia, Achilles' tendon, gastrocnemius, and soleus are emphasized in every treatment protocol.
If the pain is not relieved by conservative treatment, then extracorporeal shock-wave therapy, botulinum toxin A, autologous platelet-rich plasma therapy, dex prolotherapy, and steroid injections are other options. Surgery is only advised in chronic conditions and if other therapies have failed. Every therapy though will need at least 6 weeks to have any effect.
Simultaneously, stretching exercises, ice packing, and heel strapping have to be done to ease the inflammation. A night splint is also helpful provided the offending activity is halted.
Surgical options include fasciotomy via endoscopy or it could also be via an open approach.
Home Treatment
Plantar fasciitis normally improves and heals on its own after a few months, with most cases resolving within a year with no treatment. Most people recover with conservative treatment such as rest, arch support from good shoes or inserts, and stretching the area, but not everyone. A physical therapy program is essential to treating and preventing this condition from recurring. Most martial artists with this condition should consider wearing a night splint.
Fighters must learn to stretch the plantar fascia with basic home exercises. Wear appropriate shoes with adequate arch support, preferably made by a podiatrist. Avoid walking barefoot, lose weight, and curtail repetitive exercises that traumatize the heel.
Emergency Treatment
This is not a medical emergency. These calcaneal spurs develop over a long period and hence can be treated conservatively.
Medical Treatment
Conservative treatments work for most people, with over 90 percent getting better without surgery. Simply resting the foot and heel for a time often results in significant improvement. Heel pain that lasts over a month may require more extensive treatment.
Heel pain that lasts over a month may require more extensive treatment. Treatments may include: physical therapy, stretching the area, exercise, shoe inserts or orthotic devices to correct biomechanical imbalances, specialty shoes to cushion and support area, over the counter pain relievers, night splints to maintain elasticity in area, or cortisone injections. If relief is not found within 9 to 12 months, surgery may be recommended to remove the bone spur.
Home Treatment
Use of orthoses and shoe inserts can help, Night splints must be used and pain relief through medication is helpful.
Metatarsalgia is a chronic condition and needs conservative treatment initially.
Physical therapy, orthoses and stretches form the mainstay of treatment. Conservative management is done with NSAIDs to control pain. Special orthotics must be worn with rocker sole modification and metatarsal pads. Any abnormal subtalar eversions must be corrected. MT pads can be of rubber, polyurethane, or silicone. A forefoot cushion or an MT bar can also help. Stretches in the physical therapy program must involve the calf muscles, ankles, toes, and the Achilles tendon.
Shoes and orthoses with good arch support are helpful. Metatarsal pads also relieve pressure and redistribute it across the joint.
Most bunions do not require medical treatment. Conservative treatment includes modifying shoes so that they’re low heeled and wide. Wearing orthoses to improve support and alignment can help. Analgesics like NSAID’s can relieve pain. Ice packs can reduce inflammation. Medial bunion pads prevent irritation in the affected joint. Performing stretching exercises can restore joint mobility.
See a doctor, podiatrist or orthopedic foot specialist if pain and/or swelling persists, keeps getting worse, disrupts ordinary activities, or if all shoes cause pain since bunions may turn into foot conditions such as bursitis, which means the protective pads around the joints become infected; hammertoe, which is when the affected toe becomes deformed; or metatarsalgia, which means the ball of the foot becomes inflamed and painful.
Pain is the guide for further treatment. If the joint still experience pain, then surgical procedures are advised. Osteotomy is a surgical procedure where the bone is cut and less adducted. A Wilson osteotomy has a straight cut. A chevron osteotomy has a wedge-shaped cut. Cuts could be made to the base, shaft, or the neck. By 12 months the hallux abductus angle is normal.
Arthroplasty relieves the pain and keeps the joint mobile. Here the joint is replaced by an implant. Hemiarthroplasty is where the toe length remains the same. There is less bone resection.
Arthrodesis is where the MTP joint is fused into the correct position. It's only done when the joint has undergone severe degeneration.
Soft tissue procedures involve soft tissue repair like the McBride procedure. In this procedure, the fibular sesamoid bone is excised.
Home Treatment
Conservative measures typically will improve bunions. These conservative steps include:

Common Treatments
In our Common Treatments section we discuss the various options and therapies available for the treatment of foot injuries.
